Clinicians and researchers in mental health are becoming increasingly aware of the urgent need for new treatments for severe psychiatric disorders. Many patients do not improve after trying several courses of conventional pharmacological and/or psychotherapeutic treatments; others cannot tolerate side effects or present issues with compliance.
For many decades, the availability of non-pharmacological somatic treatments for psychiatric disorders has been very limited. Fortunately, this situation is now changing rapidly as a result of our increased understanding of the neural circuitry and neurobiology of mental illnesses. Indeed, new brain stimulation techniques are quickly emerging as highly-promising novel avenues for treating a number of psychiatric disorders by “stimulating” specific brain regions with the goal of clinical improvement.
Research in this field is expanding quickly, and there are signs that the first two decades of the current millennium could well be the decades of "brain stimulation in psychiatry”.
Some brain stimulation methods, such as repetitive transcranial magnetic stimulation (rTMS), are already officially approved for clinical use and are thus available in several academic centres worldwide; others, such as transcranial direct current stimulation (tDCS) and deep transcranial magnetic stimulation (DTMS), are currently being studied extensively and will potentially become available for clinical use within the next few years.
How does brain stimulation work?
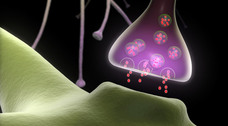
The human brain is enormously complex. One hundred billion neurons with 100 trillion connections sense, analyze, and respond to the environment. All of this interaction is done with a combination of electrical and chemical communication. Each bit of information is transformed into an electrical impulse that travels to a neuronal synapse where it is responsible for releasing chemicals into the synaptic cleft.
In other words, the brain, in fact each neuron, constantly converts electrical information to chemical signals, and then back again into more electrical information. The brain is thus an “electrical organ,” and electricity is its “currency”.
Non-invasive brain stimulation methods take advantage of the brain’s “electrical properties” by inducing weak electrical currents on its cells and indirectly causing localized neurochemical changes. This is achieved by applying electrodes or magnetic coils to a person’s scalp. Consequently, neuromodulation is often capable of “re-adjusting” the physiological activity of specific brain areas that are not as functional as they should be due to a psychiatric disorder.
Undoubtedly, knowledge about neuromodulation is likely to grow substantially in the coming years. New delivery methods, wider applications of existing technologies, and better understanding of the neural mechanisms of brain stimulation will improve the safety and efficacy of neuromodulatory treatments and contribute to a better understanding of the underlying neurobiology of psychiatric disorders.
Marcelo Berlim, MD